As the Delta variant of SARS-CoV-2 sweeps across Asia, researchers are increasingly concerned about COVID-19 spreading beyond urban centres to rural regions that were largely spared in earlier waves of the pandemic and have less access to testing, health care and vaccines.
“If the variants of concern, in particular Delta, reach far-flung areas, it will really challenge the health-care system,” says Cynthia Saloma, a molecular biologist at the University of the Philippines Diliman in Quezon City, who heads the Philippine Genome Center. Saloma says so far only a few cases of Delta have been sequenced in the Philippines, but the country is preparing for the worst. “The picture that is emerging in our neighbouring countries is really scary. We are all concerned.”
Research from India now suggests that during the nation’s brutal second wave earlier this year, the virus achieved much greater spread, beyond the urban sprawl, than during the first wave of 2020. This year’s surge was largely driven by the Delta variant, which first came to scientists’ attention in India in December.
“The variant is so much more transmissible, that health systems get overwhelmed with no time to prepare,” says Ramanan Laxminarayan, an epidemiologist at Princeton University, New Jersey, who is based in New Delhi. “The second wave has been absolutely devastating in rural India.”
Rural impact in India
From Indonesia and Malaysia to Thailand and Bangladesh, countries across Asia have detected Delta in their communities, and many are experiencing their largest outbreaks yet. In Indonesia, where confirmed cases hit 50,000 per day in mid-July, daily deaths have now surpassed 1,700. But vaccination rates remain perilously low in many of these nations, leaving them highly vulnerable.
Researchers in India are only beginning to grasp the full scale of their second wave, which hit a peak of 391,000 recorded cases a day in early May — but this data could be crucial for understanding the risk the variant poses to neighbouring nations.
In a nationwide survey of about 28,000 people (two-thirds of whom were unvaccinated and had therefore acquired immunity from infection) in June and July this year, researchers found that 68% had SARS-CoV-2 antibodies in their blood. This represented a huge increase from the 21% with antibodies, recorded in a similar survey in December 2020 to January 2021, prior to the second wave.
Although the previous survey found higher prevalence in urban areas, the latest estimates saw little difference between the numbers in urban and rural regions, which are home to 65% of India’s population. This suggests that infections “have now penetrated very well in rural areas”, says Manoj Murhekar, director of the country’s National Institute of Epidemiology in Chennai, which co-led the June survey.
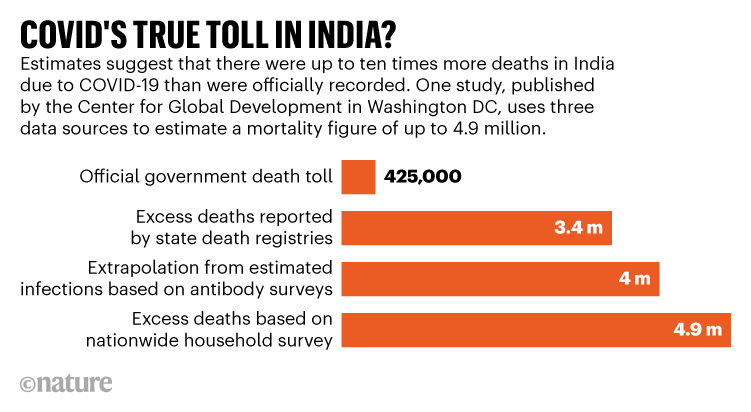
The death toll in India has been immense, and is probably much higher than official counts (see ‘COVID's true toll in India?’). Studies of excess mortality suggest that up to 4.9 million people could have died in India since the pandemic began1,2 — much higher than 425,000, the official number of recorded deaths due to COVID-19. Half these deaths probably occurred in just three months over the second wave, say researchers.
“India has definitely had a significant problem with COVID-19 mortality reporting, which is now widely recognized, and a lot of those deaths are in rural India,” says Laxminarayan.
Border regions
Researchers now fear that a similar scenario could engulf many low-income nations — in Asia and other regions, such as Africa — that also have large unvaccinated populations in rural regions with limited access to health care.
In Bangladesh, the first cases of Delta were identified in travellers from India in Dhaka and rural western districts in late April, and since then it has rapidly overtaken other variants. “It is like everything else has just disappeared,” says Senjuti Saha, a molecular geneticist at the Child Health Research Foundation in Dhaka.
Daily case numbers in Bangladesh have now hit an average of around 14,000, with daily deaths at a high of more than 230. “The numbers are bonkers,” says Saha.
Most surprising to her has been the current outbreak’s persistence in rural regions. “This totally new population is getting affected, who have been protected for whatever reason all this time,” she says.
Previous outbreaks in Bangladesh were largely restricted to cities such as Dhaka and Chittagong, despite people frequently travelling from cities of work to their families in rural regions, says Saha. This could be due to the lower population density outside cities and the outdoor lifestyle in those places, she speculates. But in this latest surge, rural regions appear to be no barrier to Delta.
Lack of access to healthcare
The trend will make the pandemic much harder to control in Bangladesh, where health-care and testing facilities are concentrated in large cities, says Saha.
In Indonesia, which is experiencing a massive second wave, researchers are worried about the spread of COVID-19 to remote parts of the nation.
Bimandra Djaafara, an infectious-diseases epidemiologist at Imperial College London who has modelled the pandemic in Indonesia, worries about a “lack of access to healthcare facilities and oxygen, especially in rural areas and areas outside Java with poorer facilities”.
Henry Surendra, an epidemiologist at the Eijkman–Oxford Clinical Research Unit in Jakarta, is concerned about the risk of death in children in rural regions of Indonesia. In a study last year3, he found that about 10% of young children hospitalized for COVID-19 in Jakarta died of the disease. But even before the pandemic, child-mortality rates were higher in rural areas because of malnutrition and diseases such as malaria and tuberculosis. Children who already had other health problems could be at even higher risk of death from COVID-19, he says.
Charting the spread
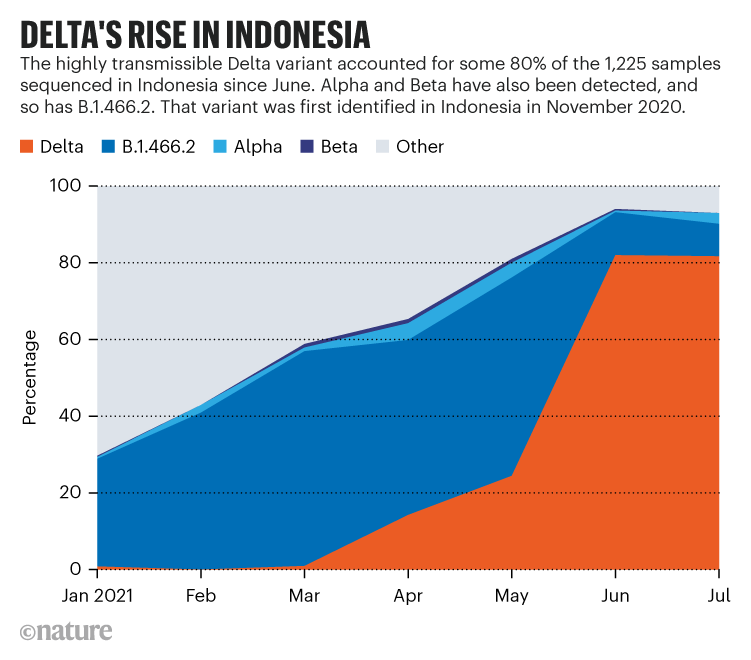
Delta has been detected in almost every province in Indonesia, and now makes up some 80% of all sequenced samples (see ‘Delta’s rise in Indonesia’). However, with limited genomic sequencing — especially in rural areas — tracking its spread has been challenging, says Safarina Malik, a molecular biologist at the Eijkman Institute for Molecular Biology in Jakarta.
The large majority of Indonesia’s 3,900 fully sequenced genomes — a tiny fraction of the confirmed cases — are from Jakarta and the surrounding island of Java, with only one sample each from the northeastern provinces of Maluku Utara and Papua Barat. Sending samples to Java for sequencing can be tricky, says Malik, as airlines sometimes refuse to carry live virus.
Other nations have even more limited sequencing. In Bangladesh, for example, some 2,000 samples have been sequenced. Delta accounted for 89% of the 203 samples collected since June, says Marufur Rahman, a molecular biologist and physician at the Center for Medical Biotechnology in Dhaka. Delta has been isolated in 43 of 64 districts, but has likely extended beyond these regions as samples are not collected from all districts, says Rahman.
The Delta variant isn’t the only reason for the pandemic’s spread beyond urban centres, say researchers. Djaafara found that strict travel restrictions in Indonesia during Ramadan and Eid in 2020 helped to contain the spread of COVID-19 to rural parts of Java4. But cases were higher and movement was much less restricted during this year’s Eid holidays in July, he says.
In Bangladesh, too, a huge number of people this year travelled for the Eid holidays despite restrictions, says Rahman.
Vaccine gap
The rise of Delta in India and now nations across Asia highlights the crucial role of vaccination in stemming the pandemic, says Laxminarayan. “Delta just increases the vulnerability of countries that have poor vaccination coverage,” he says.
In Bangladesh, close to 6% of the population has received at least one dose of vaccine. In the Philippines, that figure is 11%. Indonesia has vaccinated some 17%, but most doses have gone to the more populated islands of Java and Bali, and getting doses to the nation’s thousands of smaller islands will be logistically difficult, say researchers.
Malaysia, where there are more than 16,000 new cases of COVID-19 each day, is in a slightly better position. Yoke-Fun Chan, a virologist at the University of Malaya in Kuala Lumpur, says the country is “aggressively vaccinating”: so far, 45% of its population is partially or fully vaccinated. “Rather than looking for the virus, now we are looking for solutions to stop the virus,” she says.
Although India serves as a warning to nations with large rural and remote populations, cities remain at risk across the developing world, too. In Indonesia, “the concern is not only that it could reach rural areas, but also what is happening in the big cities”, says Malik.
In May, Thailand detected its first cases of the Delta variant in Bangkok. Numbers have since surged to new heights, spilling to cities nationwide.
Part of the reason Thailand was able to maintain relatively low case numbers in previous waves of the pandemic is “because most of the outbreaks were not in Bangkok”, says Surakameth Mahasirimongkol, director of the departments of medical life sciences and genomic medicine at Thailand’s Ministry of Public Health. But Delta has now arrived in the heart of the capital and is proving very difficult to contain, he says.
"that" - Google News
August 06, 2021 at 06:41AM
https://ift.tt/3rUzBGk
Delta threatens rural regions that dodged earlier COVID waves - Nature.com
"that" - Google News
https://ift.tt/3d8Dlvv





Tidak ada komentar:
Posting Komentar